Chronic Kidney Disease (CKD)
Introduction
Chronic kidney disease is defined as sign of kidney damage or decreased glomerular filtration with a duration of 3 months. All disease processes involving the kidney will, in principle, could lead to chronic kidney disease. Population studies have shown that over 10% of Norway's adult population suffers from chronic kidney disease. Renal failure in all stages is a strong risk factor for cardiovascular disease and death. Most patients with CKD will never find time to symptomatic kidney failure or kidney failure in end stage disease (ESRD). Since CKD is asymptomatic until advanced stages of the disease is highly dependent on actively look for at-risk individuals to detect sykdomsproseser kidneys early and thus could prevent the progression of kidney disease and cardiovascular disease episodes. Causes
The prevalence of chronic kidney disease increases with increasing age. Hypertension and diabetes are the most common causes of ESRD in the Western world, while glomerulonephritis and tubulo-interstitial diseases account for a smaller share. All disease processes that affect the kidneys including chronic diseases of other organs, may cause chronic kidney disease. A broad study including renal biopsy is therefore often necessary to determine the underlying mechanism behind the chronic kidney disease. Clinical presentation and staging
Symptoms early stage is dependent on the underlying disease. Symptoms due to reduced renal function often comes late in the course. When the GFR falls below 50-60 ml / min will apply blood deviation, while uremic symptoms often do not apply before GFR falls below 20 mL / min. Uremic symptoms are nonspecific, how asthenia, weight loss, itching and loss of appetite are the classic. To early identify patients with CKD must therefore actively look for disease in at-risk individuals. Nyresykdom stadieinndeles ut fra GFR, som kan estimeres ut fra pasientens serum kreatinin, hvor formler korrigerer for alder, kjønn og etnisitet. Hvis GFR er under 60 ml/min/1,73 m2, har pasienten nyresykdom og andre kriterier trengs ikke for å påvise nyresykdom.
Hvis GFR er over 60 ml/min/1,73 m2, må pasienten i tillegg ha andre tegn på nyreskade. I all hovedsak dreier dette seg om strukturelle avvik på UL eller patologisk proteinekskresjon i urinen.
Å identifisere en pasient med nyresykdom er derfor enkelt og lite kostnadskrevende, serum kreatinin og urinundersøkelse med mikroskopi og albumin/kreatinin ratio vil fange det store flertallet av pasientene med nyresykdom.
Stadieinndeling:
| Stadium | GFR ml/min/1,73m2 | Beskrivelse |
| 1 | >90 | Normal nyrefunksjon, men strukturelle avvik eller urinfunn tyder på nyresykdom |
| 2 | 60-89 | Lett redusert nyrefunksjon, strukturelle avvik eller urinfunn tyder på nyresykdom |
| 3A | 45-59 | Moderat redusert nyrefunksjon |
| 3B | 30-44 | Moderat redusert nyrefunksjon |
| 4 | 15-29 | Alvorlig redusert nyrefunksjon |
| 5 | <15 | Nyresykdom i sluttstadiet |
For å bedre karakteriere pasientene benyttes suffikser etter den GFR
baserte stadieinndelingen for å indikere proteinuri, transplantatnyre
og dialyseavhengighet.
Suffikser:
| p | indikerer signifikant proteinuri > 500 mg/døgn. Proteinuri er en uavhengig risikofaktor både for progresjon av nyresykdom og kardiovaskulær risiko. Signifikant proteinuri indikerer derfor en pasient med høyere riisko enn uten proteinuri. |
| T | indikerer at pasienten har nyretransplantat. |
| D | Indikerer at pasienten er i dialyse og skiller de i
stadium 5 som er får dialyse fra de som ikke får dialyse. |
Eksempler:
Pasient med GFR 50, signifikant proteinuri: Stadium 3Ap
Transplantert pasient med GFR 50 og signifikant proteinuri: Stadium 3ATp
Course and treatment
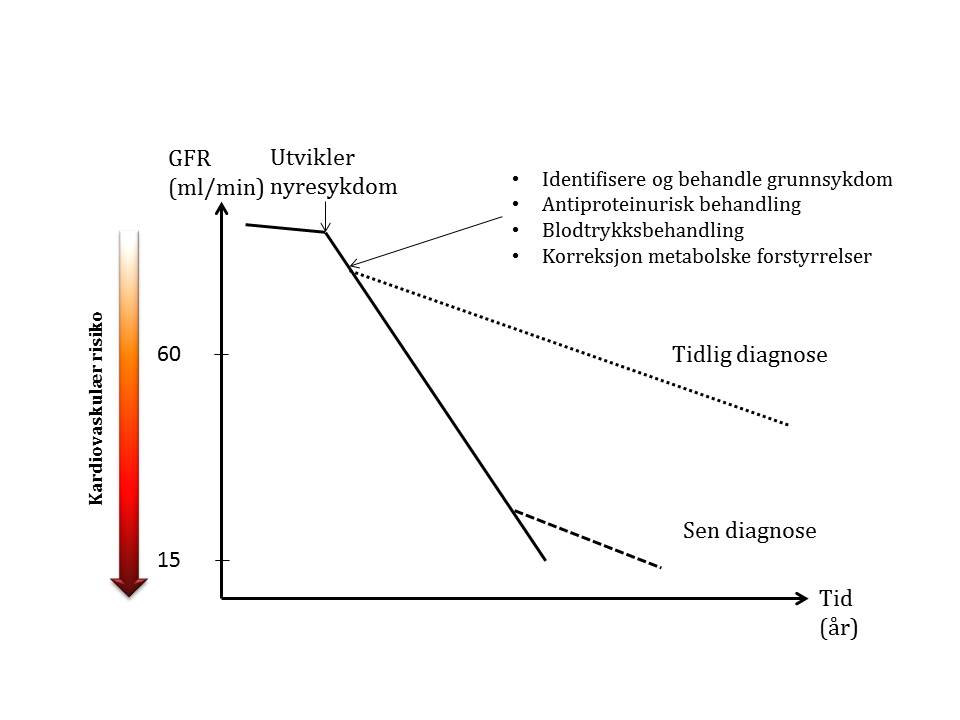
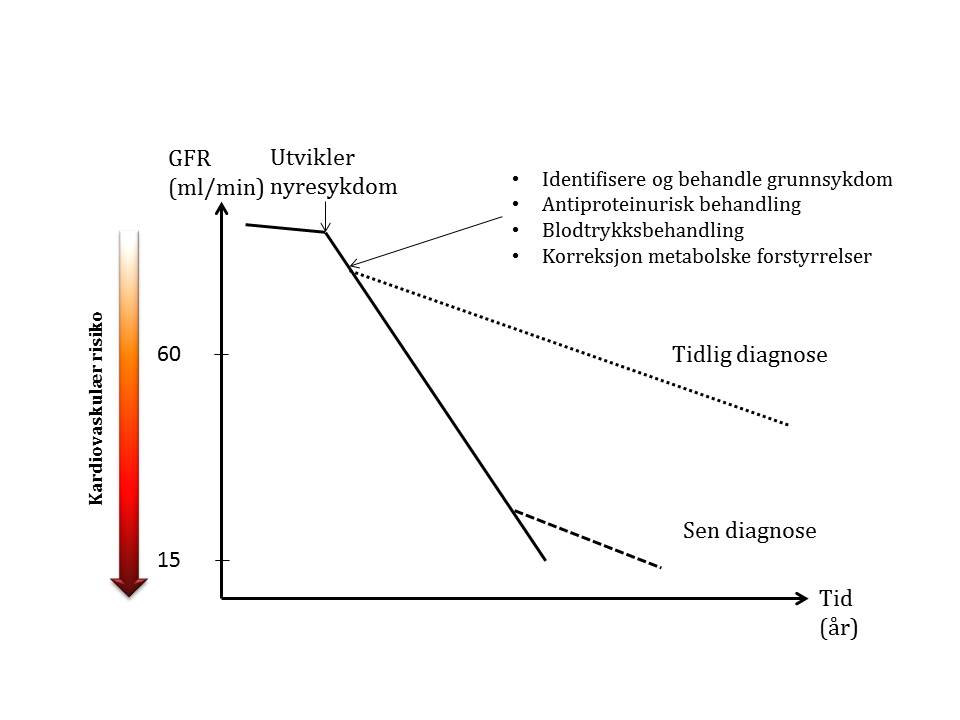
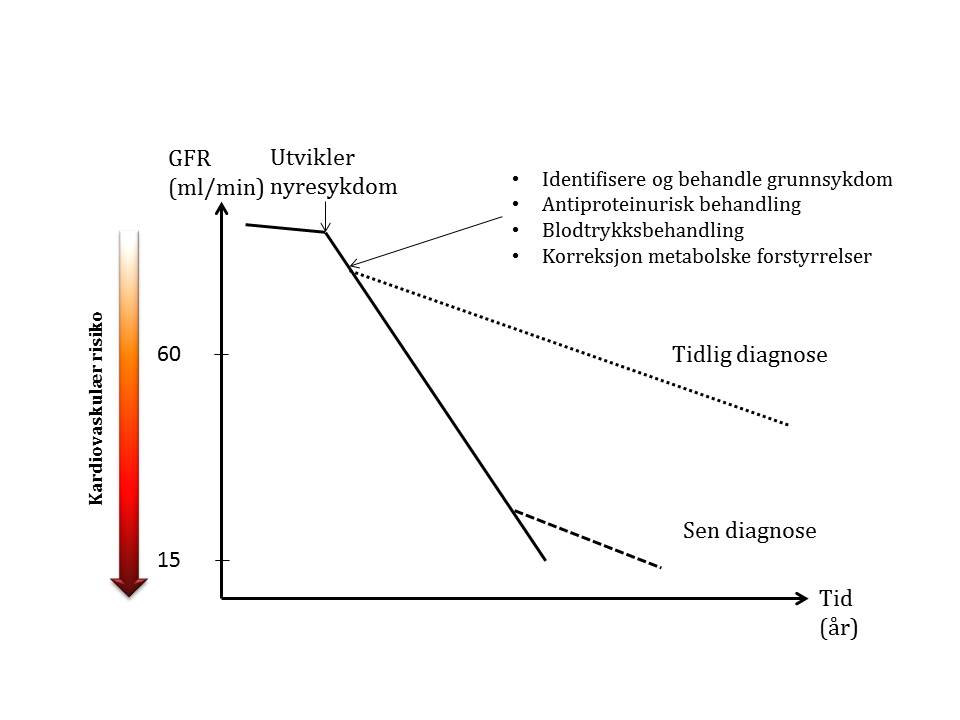
When a patient develops CKD will GFR loss per unit time increase depending on the kidney disease he develops. Adequate treatment of the underlying disease, antiproteinurisk treatment and blood pressure treatment with correction of metabolic disorders can slow the loss of GFR. It is therefore important to early detection that measures can provide a substantial postponement of the need for renal replacement therapy and at least as important for preventing cardiovascular disease in which the risk rises abruptly by declining GFR.