The most common drugs that cause kidney damage
In theory, ALL drugs can lead to acute tubulointerstitial nephritis and kidney damage. On the other hand, there are some drugs and substances used for diagnostics that one should be aware of as they have a higher risk of kidney complications.
Aminoglycosides
As a class of drugs, antibiotics are the most common cause of drug-induced kidney damage due to widespread use. Aminoglycosides make up a significant part of these and 7-36% of patients that use the drug are found to have effects on their kidneys. This has resulted in a decreased use of this medicine. Aminoglycosides are not bound to proteins and are freely filtered in the glomeruli, renal elimination is the most important method of elimination. They accumulate in tubulus cells and likely have direct toxic effects that lead to acute tubular necrosis (ATN). The duration of treatment and concentration are important parametres in toxicity levels and must be monitored. Like in other cases of ATN, the kidney damage is reversible if the medicine is discontinued in time, but it can take many weeks before the kidney function recovers.
Penicillins/cephalosporins
These antibiotics can result in an acute tubulointerstitial nephritis. The classical hypersensitivity triad of feber, rash, and eosinophilia together with acute kidney failure occurs in about 1/3 of patients with an acute TIN triggered by these drugs.
NSAIDs
NSAIDS are amongst the most commonly used medicines in the clinical practice. They can potentially affect the kidneys in multiple different ways that present differently in the clinic.
Renal prostaglandins are important in the regulation of blood flow through the kidneys. In instances with reduced effective circulating volume (hypovolemia, heart failure, cirrhosis etc.), the blood flow through the kidneys is dependent on the vasodilating effects of the prostaglandins. NSAIDS inhibit these effects and can therefore lead to acute kidney failure on the grounds of haemodynamics.
NSAIDs are also an important cause of acute tubulointerstitial nephritis. However, the clinical presentation differs from the classical acute TIN by f.ex antibiotics because eosinophilia is less common, and the changes in the glomerulus, as seen with minimal change nephropathy, can lead to interstitial nephritis and thereby nephrotic proteinuria. Furthermore, the condition can occur up to one year after the exposure to the medication, longer than normal for acute TIN.
Prostaglandins are also involved in the homeostasis of sodium, potassium and water. NSAIDs can therefore result in edema, hyperkalemia and hypertension.
Lastly, NSAIDs are also a causal factor for chronic TIN together with other analgesics.
Radiocontrast
Contrast dye induced nephropathy is a common cause for acute kidney failure among hospitalised patients. Patients with chronic kidney disease have an increased risk of nephropathy from radiocontrast containing iodine. Older patients and those with heart failure are thus at risk. Creatinine begins to rise during the first 24 hours and peaks within 2-5 days. It is normally reversible within the first 14 days. Even though the damage is reversible, it is associated with increased mortality and susceptible patients may temporarily require dialysis. Contrast dyes damage kidneys through multiple mechanisms. Reduced renal blood flow, due to constricting the afferent arteriole, and redistribution of the post-glomerular blood flow results in renal medullary ischemia. The toxic effects of the contrast dye on the cells in the tubule, together with the ischemia, result in damage to the kidney. Adequate intravenous hydration of patients at risk will help prevent nephropathy. Nevertheless, in patients with chronic kidney disease, all contrast imaging must be well-founded and without a good alternative.
Lithium
Lithium is one of the most effective treatments for bipolar disorder. There are many kidney syndromes, including nephrogenic diabetes insipidus, that can be irritating in 20-30% of patients treated with lithium. Long term use of lithium is also related to chronic tubulointerstitial nephritis, and rare cases of FSGS have also been described. (Read more about lithium nephropathy, intern lenke)
ACEi/ARB
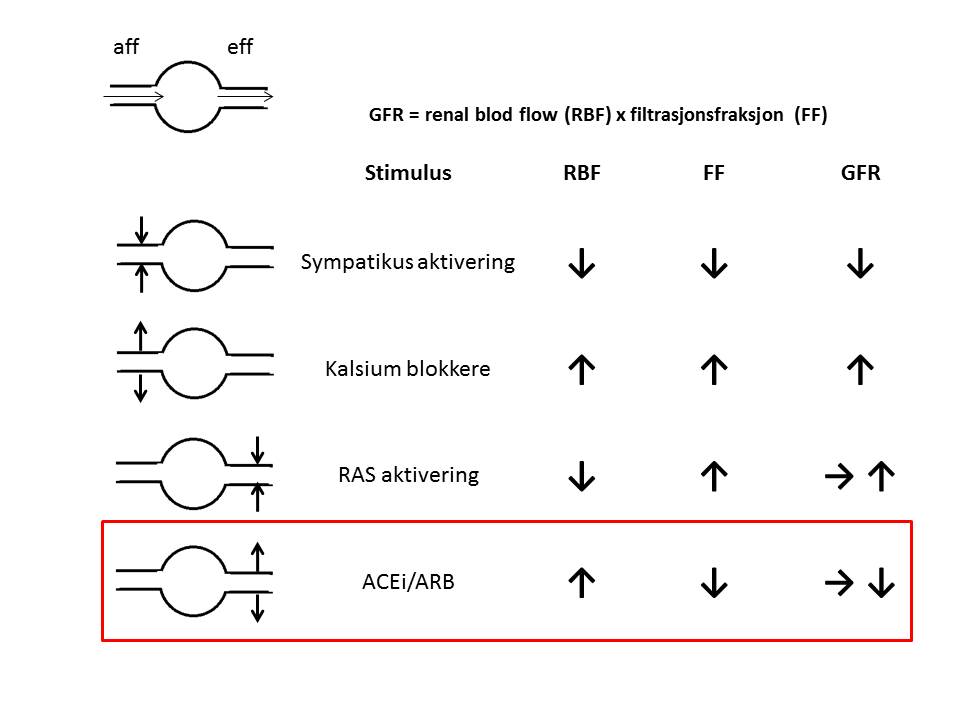
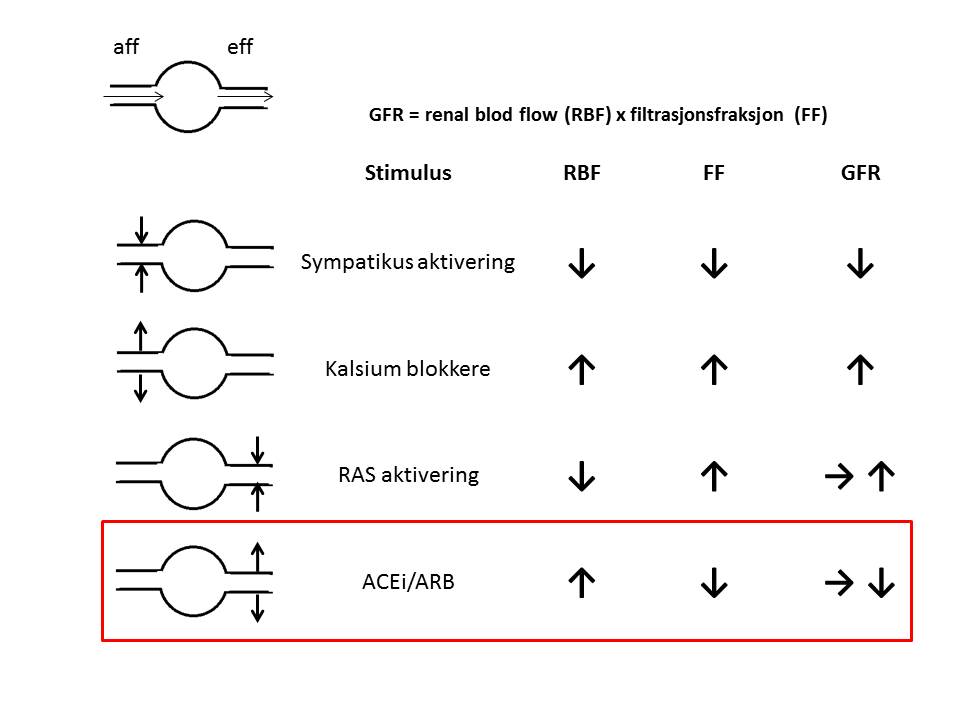
Inhibitors of angiotensin converting enzyme (ACEi) and angiotensin II receptor blockers (ARB) are blood pressure medications that inhibit the renin-angiotensin system (RAS). These drugs are commonly prescribed to patients with kidney disease as they are also antiproteinuric and renoprotective by improving the renal blood flow and decreasing the glomerular filtration pressure.
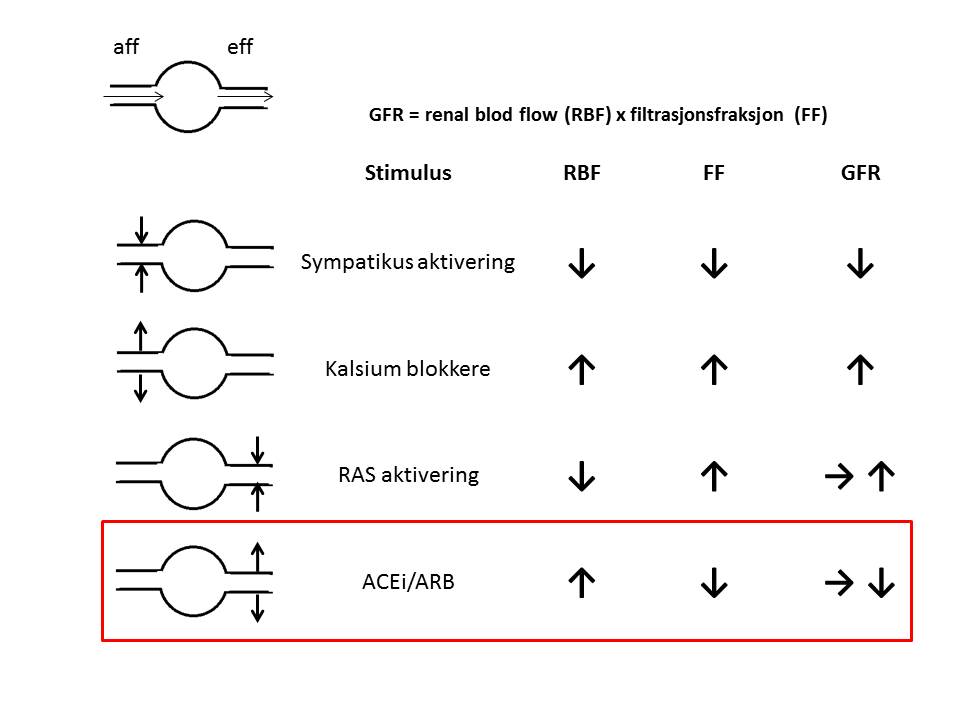
In a marginal renal blood flow condition, the kidney is dependent on RAS to maintain the GFR. In such a case, the use of ACEi and ARB can lead to severe acute cases of kidney failure. If creatinine rises under ACEi/ARB treatment, one should attempt to find the cause of the reduced renal blood flow. Because the medications are so important for maintaining GFR for as long as possible, possible causes of reduced renal blood flow should be reversed before concluding that the patient does not tolerate the medication. Dehydration due to diarrhoea or use of diuretics, infectious conditions, hypotention and stenosis of the kidney arteries are all potentially reversible causes that should be considered. Temporary reduction of the dosage or discontinuing the treatment may be necessary in the acute phase, with reintroduction of the drugs in a stable phase.
It is therefore partly a misunderstanding that ACEi/ARB are nephrotoxic and that one should be careful with these medications in those with kidney disease or reduced kidney function. Essentially, they are important renoprotective medications, especially for proteinuric kidney diseases.