Chronic kidney disease (CKD)
Introduction
Chronic kidney disease is defined as signs of kidney damage or reduced glomerular filtration rate lasting more than 3 months. All diseases involving the kidneys can in theory lead to chronic kidney disease. Population studies have shown that over 10% of adults in Norway suffer from chronic kidney disease. Kidney failure in all stages is a strong risk factor for cardiovascular disease and death. The majority of patients with CKD will not make it to symptomatic kidney failure or end-stage renal disease (ESRD). Since CKD is asymptomatic up to advanced stages of the disease, one is dependent on actively searching patients at risk to diagnose diseases early and thereby be able to prevent progression of the disease and episodes of cardiovascular disease.
Causes
The prevalence of chronic kidney disease increases with age. Hypertension and diabetes are the most common causes of ESRD in the western world, while glomerulonephritis and tubulointerstitial diseases play a smaller role. All diseases that affect the kidneys, including chronic diseases in other organs, can result in chronic kidney disease. A broad investigation including kidney biopsy is often necessary to diagnose the underlying mechanism of the chronic kidney disease.
Clinical presentation and staging
The syptoms in the early stages are dependent on the underlying disease. Symptoms that result from reduced kidney function often occur in the later stages. When the GFR is under 50-60 ml/min, deviations in the blood tests occur, while uremic symptoms often do not appear before the GFR is under 20 ml/min. Uremic symptoms are nonspecific, where the classical symptoms are asthenia, weight loss, itching and reduced appetite.
Therefore, in order to identify CKD in patients early, one must actively search for the disease in individuals at risk.
Kidney diseases are classified based on the GFR which can be estimated from the patient's serum creatinine, corrected for age, gender and ethnicity. If the GFR is under 60 ml/min/173 m2, the patient has kidney disease and no other criteria is needed to diagnose kidney disease.
If the GFR is over 60 ml/min/1,73 m2, the patient must have additional signs of kidney damage. These are mainly structural abnormalities seen on ultrasounds or pathalogical protein excretion in the urine.
Therefore, identifying a patient with kidney disease is simple and cheap. Serum levels of creatinine, microscopy of urine, and the albumin/creatinine ratio will identify the majority of patients with kidney disease.
Classification:
| Stage | GFR ml/min/1,73m2 | Description |
| 1 | >90 | Normal kidney function but with structural abnormalities or markers in the urin pointing toward kidney disease |
| 2 | 60-89 | Slightly reduced kidney function, structural abnormalities, or markers in the urin pointing toward kidney disease |
| 3A | 45-59 | Moderately reduced kidney function |
| 3B | 30-44 | MModerately reduced kidney function |
| 4 | 15-29 | Severely reduced kidney function |
| 5 | <15 | End-stage kidney disease |
In order to better classify patients, suffixes after the GFR-based staging are used to indicate proteinuria, transplanted kidneys and dependence on dialysis.
Suffixes:
| p | indicates significant proteinuria > 500 mg/day. Proteinuria is an independent risk factor for both the progression of the kidney disease and risk for cardiovascular disease. Significant proteinuria is therefore an indicator for patients with higher risk than those without proteinuria. |
| T | indicates that the patient has a kidney transplant. |
| D | indicates that the patient is undergoing dialysis and divides those in
stage 5 who receive dialysis from those who do not. |
Examples:
Patient with GFR 50, significant proteinuria: Stage 3Ap
Transplanted patient with GFR 50 and significant proteinuria: Stage 3ATp
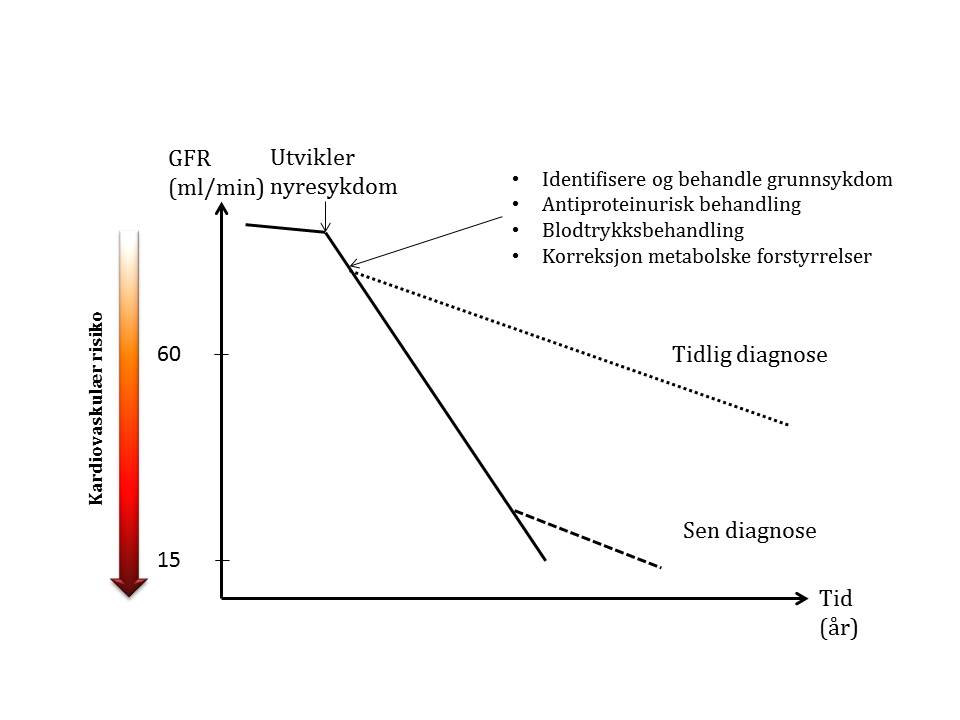
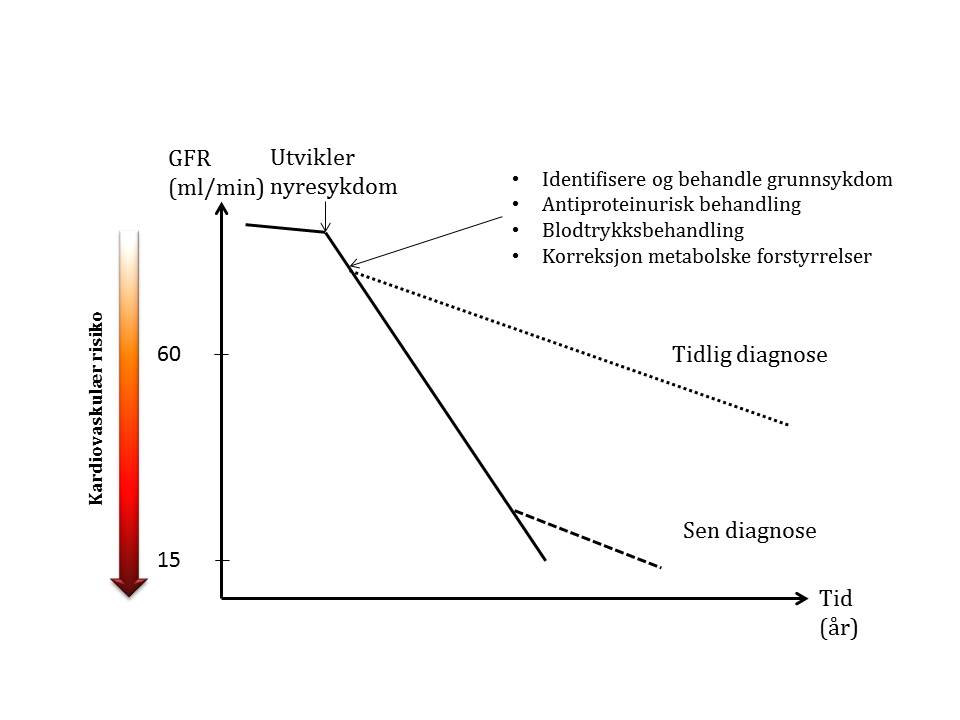
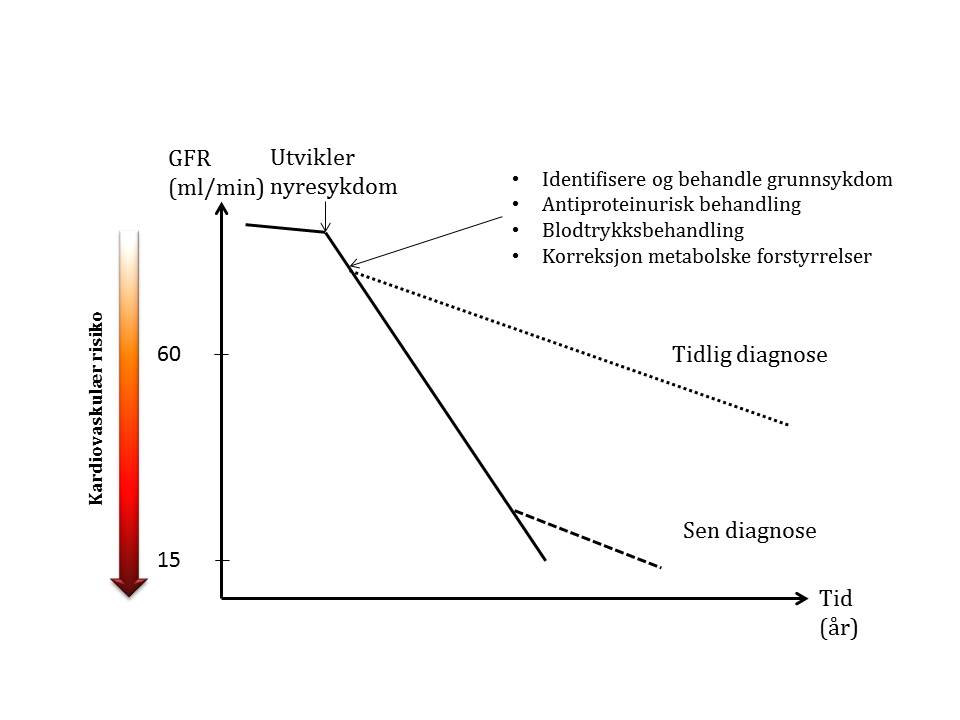
Prognosis and treatment
When a patient develops CKD, the fall in GFR per unit of time will increase dependent on which kidney disease has developed. Adequate treatment of the underlying disease, proteinuria, and hypertension, together with correction of metabolic imbalances can slow down the fall in GFR. It is therefore important to diagnose the disease early so that the measures can result in a significant delay in requiring renal replacement therapy. And of equal importance is preventing cardiovascular disease where the risk increases sharply with falling GFR.